Search
closeNetwork updates for some GEHA members
Effective Jan. 1, 2024, Government Employees Health Association (GEHA) members in the following states will now access the Choice Plus health care professional network* if they’re enrolled in the standard option, high option or high deductible health plans:
Alaska
Arizona
Colorado
Connecticut
Georgia
Kentucky
Maine
Massachusetts
Michigan
Nevada
New Hampshire
New Jersey
New York
Ohio
Pennsylvania
Rhode Island
Utah
Vermont
Washington
What this means for you
Some of your patients may be GEHA members in 2024. You do not need to take any action during this transition. You can recognize GEHA members by looking at the member ID card:
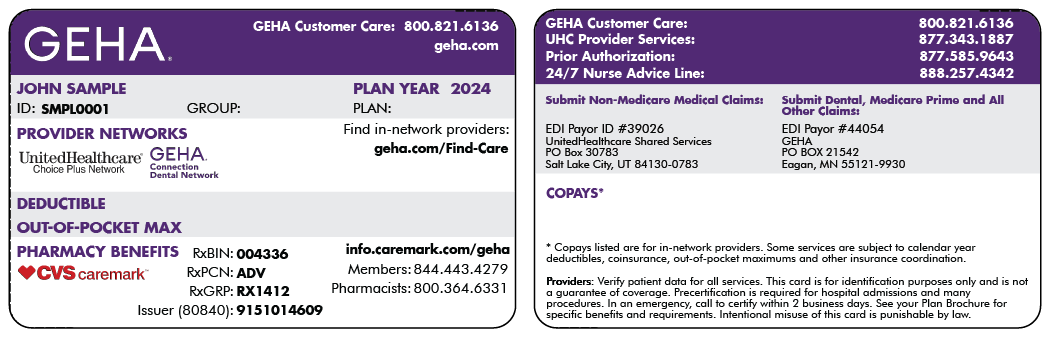
Sample member ID card for illustration only; actual information varies depending on payer, plan and other requirements.
GEHA members with the Choice Plus and Select Plus network will have:
- Access to our national UnitedHealthcare network of health care professionals and facilities
- Medical and mental health utilization management (UM) services, including notification, initial determination and inpatient care management
- Access to the UnitedHealthcare Behavioral Health network and mental health, behavioral health and substance use disorders UM services
Questions?
Check the member’s ID card for contact information. For eligibility, summary of benefits, prior authorization requirements and claim status, call Provider Services at 877-343-1887 or visit uhss.umr.com.
*This change does not impact GEHA members on policy 918695, Surest policy 78800521 or Medicare Advantage (PPO) Group Numbers 16610 and 16611.
PCA-1-23-02919-UHN-NN_11092023