Surest Health Plan Information for Providers
Surest is a UnitedHealthcare company that administers a health plan without a deductible or coinsurance.
If you’re a participating health care professional for UnitedHealthcare commercial plans, you automatically participate in our Surest™ benefit plans.
Surest is a UnitedHealthcare company that administers a health plan without a deductible or coinsurance. Members have access to the nationwide UnitedHealthcare and Optum® Behavioral Health networks and can check costs and care options in advance.
A small number of members have the Surest Flex plan, which includes the feature of flexible coverage. For a fixed list of plannable tests, procedures or treatments, the member must activate coverage at least 3 business days in advance of the service, or the member may not have coverage for the service. Visit the Surest Provider Guide to learn about flexible coverages.

Use EDI to get variable copay amounts
Add practitioner and location data to your 270 inquiry and you’ll get accurate 271 copay amounts in our enhanced Electronic Data Interchange. See what fields to enter.

Actions you can take in the portal
Sign in to the UnitedHealthcare Provider Portal to review your claims, verify member eligibility and check variable pricing.

Interactive guide
Explore this self-paced guide for everything you need to know about working with Surest benefit plans.

Register for an upcoming webinar
Join a live webinar to get important Surest information on the spot and participate in interactive, chat-based Q&As.
Member ID card examples
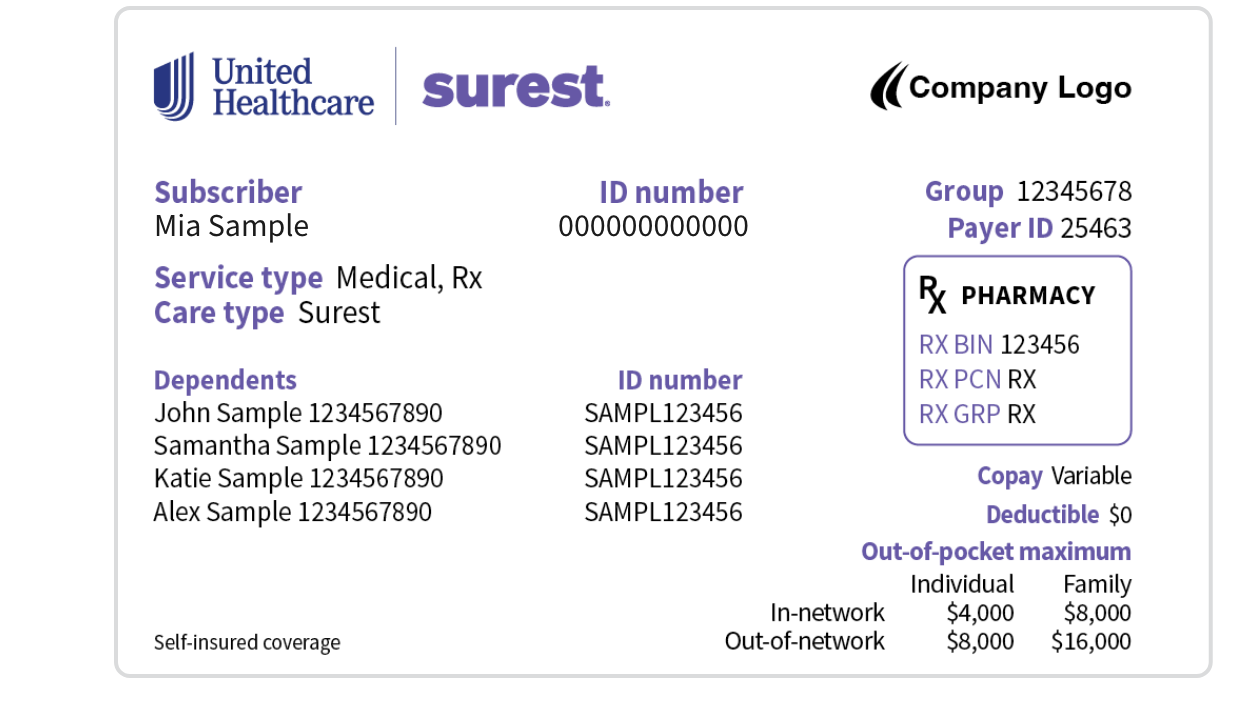
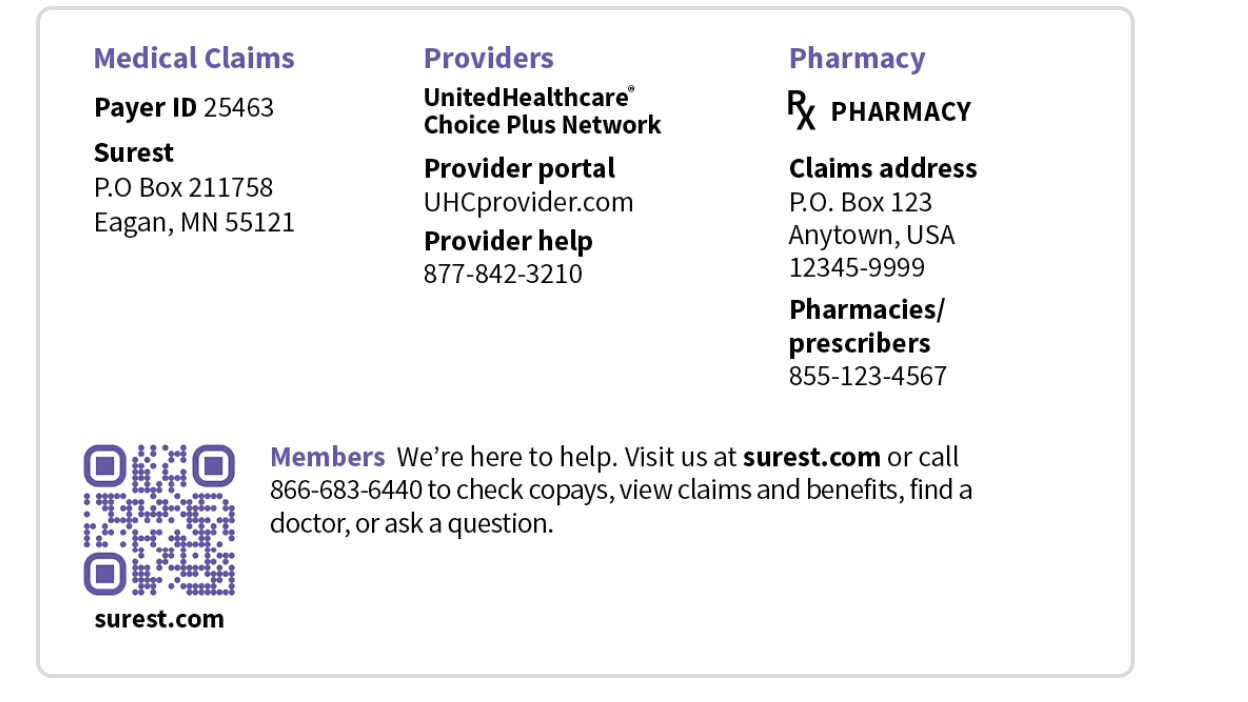
Sample member ID card for illustration only; actual information varies depending on payer, plan and other requirements.
Surest payer ID and address
- For digital claims, use 25463
- For paper claims, mail to Surest at P.O. Box 211758, Eagan, MN 55121
Please include the subscriber ID and rendering address on claims to help us confirm the copay/member price.
Frequently asked questions
To help ensure pricing reflects the best and most recent data, member copays/prices are updated annually. Accordingly, you always need to check the current member copay/price before collecting payment for a service. Although a service's member copay/price may change, your contracted rate for the service doesn’t.
Note: Member copays/prices for a service can vary by facility and/or health care professional.
For members with Surest Flex plans, a small set of plannable procedures and treatments require the member to activate coverage at least 3 business days in advance or they won’t have coverage for the treatment. You should confirm the member’s eligibility and benefits and that the member has activated coverage for a service in advance for certain treatments or procedures.
The prior authorization/notification requirements in the UnitedHealthcare Administrative Guide apply to Surest Flex plans. These are services for which the member must activate coverage for certain plannable procedures or treatments at least 3 business days in advance.
For more information, visit our Advance Notification and Clinical Submission Requirements page and select Surest Health Plans Advance Notification/Prior Authorization Requirements.
Manage Surest tasks online and find information related to eligibility, claims and prior authorizations using the portal, Application Programming Interface (API) or Electronic Data Interchange (EDI). For more information, see our Digital Solutions page and the 270/271 EDI Surest guide.
Please submit claim reconsiderations in the portal by clicking Sign In at the top right of this page. For more information, see our Claims reconsideration quick start guide.
Or, send claim reconsiderations by mail to:
Mail: UHSS, Attn: Claims, P.O. Box 30783, Salt Lake City, UT 84130
Fax: 866-427-7703
If applicable, please send the claim to the attention of the representative you spoke with.
Note that clinical appeals are only for services that received a medical necessity review and weren’t determined to be medically necessary.
Please send clinical appeals to:
Mail: Surest Appeals, P.O. Box 31270, Salt Lake City, UT 84131
Fax (non-urgent): 866-748-7820
Fax (urgent): 866-748-7304
Remember to provide all supporting materials in your appeal, including member-specific treatment plans and clinical records.

Resources
- Surest Provider Guide
- Surest resources for providers
- Surest supplement in the UnitedHealthcare Administrative Guide
- Surest survey to provide your feedback on working with the health plan
- Surest helpful tips and resources 1-page guide

Questions?
- Visit Surest Provider Services
- Connect with us through chat 24/7 in the UnitedHealthcare Provider Portal
- Call the Provider Services number on the member’s ID card


